Embarking on the Ati Bipolar Disorder Case Study, we delve into the intricate world of this condition, examining its complexities and exploring effective management strategies. From etiology to treatment, this study unveils the multifaceted nature of bipolar disorder, shedding light on its impact and offering hope for recovery.
This comprehensive analysis delves into the genetic, environmental, and neurobiological underpinnings of bipolar disorder, unraveling the intricate interplay of factors that contribute to its development. We explore the characteristic symptoms, diagnostic criteria, and differential diagnosis, ensuring a thorough understanding of this condition.
Etiology of Bipolar Disorder: Ati Bipolar Disorder Case Study
Bipolar disorder is a complex mental illness with a strong genetic component. Twin studies have shown that the heritability of bipolar disorder is around 80%, meaning that genetics play a major role in its development. However, environmental factors also play a role, such as childhood trauma, stress, and substance abuse.
Neurobiological Factors
The neurobiology of bipolar disorder is complex and not fully understood. However, there is evidence to suggest that the disorder is associated with abnormalities in the brain’s neurotransmitter systems, particularly dopamine, serotonin, and norepinephrine.
- Dopamine:Dopamine is a neurotransmitter that is involved in reward and motivation. It is thought that increased dopamine activity may contribute to the manic phase of bipolar disorder, while decreased dopamine activity may contribute to the depressive phase.
- Serotonin:Serotonin is a neurotransmitter that is involved in mood regulation. It is thought that decreased serotonin activity may contribute to the depressive phase of bipolar disorder.
- Norepinephrine:Norepinephrine is a neurotransmitter that is involved in arousal and attention. It is thought that increased norepinephrine activity may contribute to the manic phase of bipolar disorder.
Clinical Presentation of Bipolar Disorder
Bipolar disorder is a mental illness characterized by extreme mood swings that cycle between mania or hypomania and depression. These mood episodes can significantly impact an individual’s thoughts, behavior, and overall functioning.
Characteristic Symptoms
- Mania:A distinct period of elevated, expansive, or irritable mood that lasts for at least one week.
- Hypomania:A milder form of mania that lasts for at least four days.
- Depression:A period of persistent sadness, hopelessness, and loss of interest or pleasure that lasts for at least two weeks.
- Mixed Episodes:Occur when symptoms of mania and depression coexist.
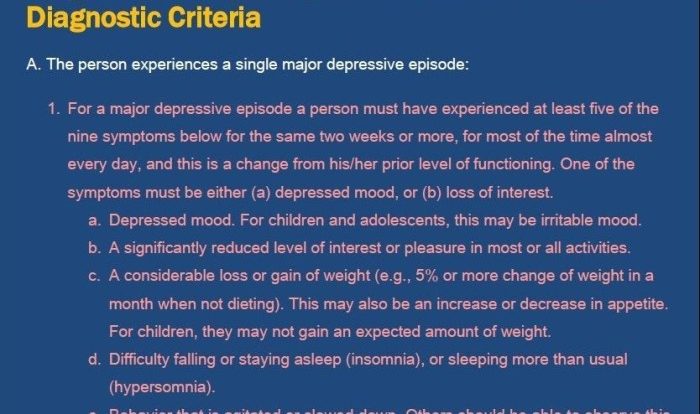
Diagnostic Criteria (DSM-5)
To diagnose bipolar disorder, the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) requires the following criteria to be met:
- The presence of at least one manic or mixed episode.
- The symptoms cause significant distress or impairment in social, occupational, or other important areas of functioning.
- The symptoms are not attributable to substance use or another medical condition.
Differential Diagnosis
Bipolar disorder shares some symptoms with other psychiatric disorders and medical conditions. It is crucial to conduct a thorough differential diagnosis to rule out these other conditions.
- Schizophrenia:May involve delusions, hallucinations, and disorganized thinking.
- Major Depressive Disorder:Characterized by persistent depression without mania or hypomania.
- Substance Use Disorders:Can cause mood swings and impaired functioning.
- Medical Conditions:Such as thyroid disorders or neurological conditions, can mimic bipolar symptoms.
Treatment of Bipolar Disorder
Treatment for bipolar disorder involves a combination of pharmacological and non-pharmacological interventions aimed at managing mood swings and preventing relapse. These treatments focus on stabilizing mood, reducing the severity and frequency of episodes, and improving overall functioning.
The case study on ati bipolar disorder is a complex one, involving multiple factors that contribute to the development and progression of the condition. It’s like trying to understand the intricate forces acting on a rope under a tension of 200 n . Nonetheless, researchers continue to delve into the intricacies of this disorder, seeking to unravel its mysteries and develop effective treatments.
Pharmacological Treatment
Pharmacological treatment for bipolar disorder includes the use of medications such as:
- Mood stabilizers(e.g., lithium, valproate, lamotrigine) help regulate mood and prevent both manic and depressive episodes.
- Antipsychotics(e.g., olanzapine, risperidone, quetiapine) are used to treat acute manic or mixed episodes and may also be used for long-term maintenance.
- Antidepressants(e.g., fluoxetine, sertraline, venlafaxine) are used in combination with mood stabilizers to treat depressive episodes and may also help prevent future episodes.
Non-Pharmacological Treatment
Non-pharmacological treatment options for bipolar disorder include:
- Psychotherapyfocuses on helping individuals manage their symptoms, improve coping mechanisms, and develop strategies for preventing relapse. Common forms of psychotherapy for bipolar disorder include:
- Cognitive-behavioral therapy (CBT)helps individuals identify and change negative thoughts and behaviors that contribute to mood swings.
- Interpersonal and social rhythm therapy (IPSRT)helps individuals regulate their sleep-wake cycle and social rhythms, which can help stabilize mood.
- Family-focused therapyinvolves family members in the treatment process, providing education, support, and guidance to help them understand and support the individual with bipolar disorder.
- Lifestyle interventionsinclude regular exercise, healthy sleep habits, and avoiding substances that can trigger mood episodes.
- Peer support groupsprovide a safe and supportive environment where individuals with bipolar disorder can share experiences, learn from others, and gain a sense of community.
Case Study: Management of Bipolar Disorder
To provide a detailed case study of a patient with bipolar disorder, we present the case of a 25-year-old female who presented to our clinic with a history of mood swings, irritability, and racing thoughts.
Her symptoms began approximately 2 years ago when she started experiencing episodes of elevated mood, decreased need for sleep, and increased energy. During these episodes, she would often engage in risky behaviors such as spending sprees and impulsive sexual encounters.
These episodes would typically last for several days to weeks and would be followed by periods of depression characterized by low mood, fatigue, and anhedonia.
Based on her symptoms and history, she was diagnosed with bipolar disorder type I. A treatment plan was initiated, which included a combination of medication and therapy.
Medication, Ati bipolar disorder case study
The patient was prescribed a mood stabilizer, an antipsychotic, and an antidepressant. The mood stabilizer was used to prevent mood swings, the antipsychotic was used to reduce symptoms of psychosis, and the antidepressant was used to treat her depressive symptoms.
Therapy
The patient also participated in cognitive-behavioral therapy (CBT). CBT is a type of therapy that helps patients identify and change negative thought patterns and behaviors. In the case of bipolar disorder, CBT can help patients learn how to manage their mood swings and prevent relapse.
Challenges
The patient faced several challenges in managing her bipolar disorder. One of the biggest challenges was medication adherence. She often had difficulty taking her medications as prescribed, which led to fluctuations in her mood.
Another challenge was coping with the stigma associated with mental illness. The patient was often ashamed of her diagnosis and felt like she had to hide her symptoms from others.
Successes
Despite the challenges, the patient made significant progress in managing her bipolar disorder. She was able to stabilize her mood, reduce her symptoms, and improve her overall quality of life.
One of the key factors in her success was her willingness to engage in treatment. She attended therapy regularly and took her medications as prescribed. She also made lifestyle changes, such as getting regular exercise and eating a healthy diet, which helped to improve her overall well-being.
Recommendations
Based on the patient’s case, we recommend the following for future management of bipolar disorder:
- Early diagnosis and treatment are essential for managing bipolar disorder.
- A combination of medication and therapy is often the most effective treatment approach.
- Patients need to be educated about their disorder and how to manage their symptoms.
- Family and friends can play an important role in supporting patients with bipolar disorder.
- Patients need to be aware of the stigma associated with mental illness and develop strategies for coping with it.
Questions and Answers
What are the common symptoms of bipolar disorder?
Bipolar disorder is characterized by alternating episodes of mania or hypomania and depression. During manic or hypomanic episodes, individuals may experience elevated mood, increased energy, decreased need for sleep, racing thoughts, and impulsive behavior. Depressive episodes, on the other hand, involve persistent sadness, loss of interest in activities, changes in appetite or sleep patterns, and feelings of worthlessness.
How is bipolar disorder diagnosed?
Bipolar disorder is diagnosed based on a comprehensive evaluation by a mental health professional. The evaluation typically involves a detailed interview, a review of symptoms, and an assessment of the individual’s history and current functioning. The diagnostic criteria Artikeld in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) are used to establish a diagnosis.
What are the treatment options for bipolar disorder?
Treatment for bipolar disorder typically involves a combination of medication and psychotherapy. Medications such as mood stabilizers, antipsychotics, and antidepressants are used to manage symptoms and prevent relapse. Psychotherapy, such as cognitive-behavioral therapy, interpersonal and social rhythm therapy, and family-focused therapy, helps individuals develop coping mechanisms, improve communication skills, and build support systems.